treatment Treatment of polytrauma is a rather complex medical problem. Full assistance to victims with polytrauma will be as effective as possible if the main principle is observed:
treatment
Treatment of polytrauma is a rather complex medical problem. Full assistance to victims with polytrauma will be as effective as possible if the main principle is observed: "Quickly, carefully, at the same time." The treatment process can be divided into 5 stages:
Stage I – prehospital
It starts from the moment of injury, corresponds to the beginning and period of traumatic disease, when compensatory and pathological processes are triggered. Assistance is provided by ambulance teams or through self-help and mutual assistance. But regardless of who provides first aid, one of its main elements is transport immobilization.
The first data on the use of immobilization for various injuries date back to ancient times. Even 3-4 thousand years ago, people performed immobilization with bandages to treat bone fractures. In the middle of the 16th century, the French surgeon Ambroise Pare used various splints to help the wounded. But for the first time, the importance of transport immobilization and the necessary functional properties of gauze bandages was provided by the founder of military field surgery N. I. Pirogov. For transport immobilization, he used starch dressings, for medical – plaster.
The use of modern tires for transport immobilization is associated with the name of Kramer, who in 1887 proposed a metal tire that quickly gained popularity in the armies of all European countries (Kramer's tire). In 1875, the English surgeon Thomas proposed a splint for transport immobilization for hip fractures, based on the principle of extraction.
The main drawback of the Thomas splint – passing the injured limb through the top ring of the splint – was solved in its variants proposed by J. Vlek and X. Lardenois by creating a split ring. In the Soviet Union, this tire was improved and modified by M.P. Vinogradov (Fig. 2.1).
In 1923, the Russian surgeon N. Diterikhs proposed an original splint for immobilizing fractures of the lower extremities, which proved to be very successful for fixing fractures of the femur, tibia and adjacent joints (Fig. 2.2). In 1934, the Dieterichs tire was improved and accepted for use in the Red Army.
Throughout the history of transport immobilization, wooden tires have been preferred. But most of them are interesting only in the historical aspect, because they are not plastic enough, they do not adhere well enough to the body and lose their properties during transportation. These include popular tyres, the tire of Sazon-Yaroshevich, Barentsevich and Kuslik, Faltin.At one time, the reticular tire of filler was widely used, but it did not have enough hardness, did not provide reliable immobilization and on the radiograph gave a thick grid, which made it difficult to recognize the fracture. In 1942, a fairly successful bus was proposed by I. M. Gindin, embodying the idea of "tires-blinds *.
Today, also the main means of transport immobilization are different types of tires. According to the principle of operation, they are divided into fixing and distraction. Transport immobilization tools can be standard, non-standard, improvised (handicraft) and using soft bandages (Dezo, Velpo, Rings Delba etc.).
Standard transport tires – These are means of immobilization that are equipped with medical institutions, ambulance and the like. These include wire
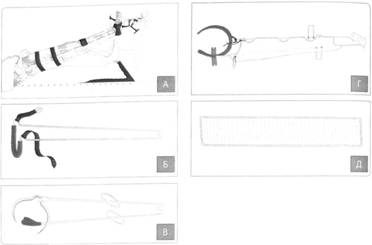
Rice. 2.1. Tires for transport immobilization:
BUT – Thomas; B. – Black; AT – Lardenua; G – Lardenoa – Vinogradova; D – stair (crater) with the possibility of modeling

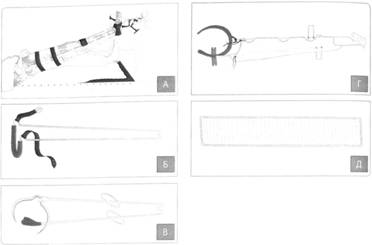
Rice. 2.2. Tire Dietershsa:
1 – Long tire board; 2. – short tire board; 2.1 – twist; 3. – Wooden sole
The staircase of the crater, distraction type of the Diterich bus, plastic tires, medical pneumatic tires (inflatable), vacuum stretchers, anti-shock costume "chestnut" (Fig. 2.3). The latter due to the pneumatic compression of the lower extremities and the lower half of the body provides a temporary stop of intra-abdominal bleeding, bleeding in the zone of bones of the pelvis, hips, legs, and the redistribution of 1.5-2 liters of blood from the depot of the lower half of the body and limbs to the central volume of blood.
Non-standard means of transport immobilization are tires and devices used in individual medical institutions or departments, but are not produced by the medical industry and non-standard tires (Elansk
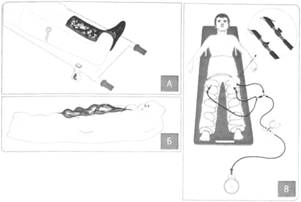
Rice. 2.3. Standard transport tires
BUT – Pneumatic medical tire; B. – Medical Pneumatic stretcher; AT – Anti-shock costume

Rice. 2.4. Elansky Bus for Transport Immobilization Head
M, Petrukhova, Bogdanova, Nechaeva, etc.) (Fig. 2.4). In the West countries, the most famous Thomas bus in the Haree modification for simultaneous immobilization and stretching and Sager bus with an extraction device.
The improvised tires are made of various primary materials on the principle of fixation tires (wooden rails, bars, bunch of branches, thick cardboard, etc.). In the absence of submitted means, you can navigate the upper limb to the body, the lower – to a healthy limb.
Regardless of the material from which the tire is made, and the conditions for its overlay, the coverage area of the limb should be sufficient for full immobilization and make up at least two thirds in circumference and two adjacent joints in length.
The algorithm for assistance in the pre-hospital stage has the following form:
• Determination of the presence of affected signs of life (consciousness, pulsation on trunk and carotid arteries, breathing)
• restoration of respiratory tract, IVL;
• Temporary stopping of bleeding, aseptic wound bandage;
• Transport immobilization of injured limbs, in the absence of special – with appliant means;
• if necessary – intubation, carrying out artificial ventilation of the lungs;
• introduction of anti-shock preparations;
• anesthesia of possible fractures
• enter into special tires of stretcher or a stretcher with a tough basis;
• to quickly deliver the victim to the medical institution.
Most of these events can be performed during the transportation of the victim in an ambulance.
Stage II – Hospital Resuscitation
Begins from the moment of receipt of the victim in the hospital and lasts up to 72 hours, that is, during the first period of traumatic disease. At this stage, the life of the victim in the counterclaim operating room is saved, which is an active tool diagnosis of damage to the method of their exceptions, restoring the vital functions of the body, to eliminate the victim from shock by conducting resuscitation activities and by performing urgent and urgent surgery. Thus, the principles of treatment of traumatic shock are the urgent nature of the provision of medical care, a differentiated approach and a leading and emergency nature of surgical treatment. It is an emergency surgical treatment that should be a pathogenetic meaning and eliminates the reason for the shock by stopping bleeding, stable fixation of long bones, eliminating the intense or open pneumothorax and the like.
Emergency operational interventions – Operations, the failure of which leads to the death of the victim, so their delay is invalid. They are performed immediately after the arrival of the victim in the medical institution, and the resuscitation measures and the diagnosis of damage are performed during operational intervention. Emergency operations in the integrated account of the joint injuries are considered as the main anti-shift event.
Urgent interventions – Operations, the failure of which threatens the life of victims, but their delay in the range of 2-6 hours is justified by the elimination of life-hazard states, preoperative preparation and instrumental diagnostics.
Upon receipt of the victim in the receiving department, the clothes are removed from it, measure AT, is carried out by sanitary processing. In this case, it is unacceptable to repeatedly translate the patient with some stretcher to others. If it allows the general state of the victim, the doctor or a brigade of the political science department examines its issue of the place, timing and procedure for examining and conducting diagnostic and therapeutic manipulations.
With a traumatic shock II-III degree of affected, they are immediately delivered to the intensive care room or in the operating room. Immediately begin to carry out anti-deposit and resuscitation activities, while at the same time conducting a review, diagnostic and therapeutic manipulations. Immediately the catheterization of the central vein, the bladder, if necessary, is intubation of the trachea.
Anti-deposit measures can be consecrated in several directions.
Recovery Usch with blood loss up to 1 l due to crystalloid and colloidal blood solutions with a total volume of up to 2-2.5 liters per day with blood loss up to 2 l – due to blood and blood substitutes in terms of 1: 2 total up to 3.5-4 liters per day with massive blood loss more than 2 l – mainly due to blood in relation to 2: 1, the total volume of the fluid may exceed 4 liters with blood loss of more than 3 l – mainly due to large doses of blood (3 l and more), while hemotransphus It is carried out by a rapid pace in two large veins or in the femoral artery. In case of intra-high bleeding, blood from the cavities need reinfusuals (with the obligatory absence of damage to the hollow organs). The rule should be compensation for lost blood during the first 2 days after injury. Effective criteria is AT stabilization, a decrease in tachycardia, restoration of red blood indicators.
Stimulation of the tone of peripheral vessels It is a prerequisite for the functioning of the heart, lungs, liver, kidneys. Effective with reduced blood loss and is performed by administering dopamine, norepinephrine at a speed of 40-50 drops per minute.
Hemodynamic stabilization With the help of glucocorticoids, which improve the contractile function of myocardium, remove the spasm of peripheral vessels, stabilize the cell membranes and reduce the permeability of the vascular wall.
Improving the rheological properties of blood With the help of rheologically active blood substitutes, crystalloid solutions, disagreganites.
Correction of blood coagulation system, which is determined by the degree of severity of the DVS syndrome. When hypercoagulation, heparin is used in a dose of 2500-5000 … 4-6 times a day, thresholdal, low molecular weight heparins. In case of hypocagulation without activation of fibrinolysis, heparin is prescribed (no more than 5000 units), prednisolone, albumin, plasma, fresh blood. When hypocoagulation with fibrinolysis activation, prednisolone, conflict, albumin, plasma, blood, fibrinogen, ditinon are used.
Metabolism correction It is the correction of acidosis, which arises, on the one hand, due to the hypoxia of tissues, and on the other – from the transfusion of a large amount of blood. Used buffer solutions of sodium bicarbonate, trisamine. With large volumes of hemotransfusion for every 500 ml of blood, it is necessary to introduce 15 ml of a 10% solution of calcium chloride.
Neutralization of enzymatic aggression It is performed by introducing enzyme inhibitors (conflict, trasilol).
Restoration and support of the kidney function. Long-term hypotension and large amounts of hemotransphus suppress the kidney function and lead to preenal renal failure, the initial manifestation of which is the level of diurus below 50 ml / hour. Stimulation begins with the introduction of saluretics (Laziks), with adequate responses to its use, hemodynamics and renal blood flow is performed by appointing rheologically active blood substitutes, disagregantes, osmotic and oncotic diuretics.
Warning of fat embolia
Preventive measures include, in addition to anti-shock, the normalization of indicators of the saturation of arterial blood oxygen, the use of fat (essences) deemulsifiers (essential), early nutritional support (the use of balanced solutions of amino acids). The main measure of prevention is the early minimally invasive synthesis of large bones (pelvis, hips, legs).
With the holding of anti-shock and resuscitation activities, diagnostic and therapeutic manipulations are carried out, emergency operational interventions.
If the patient is conscious, then, taking into account the complaints, x-ray and, if possible, instrumental examination (ultrasound, computed tomography, etc.) of these segments and systems. But in the overwhelming majority of cases, the condition of the victims does not allow additional methods of examination, therefore preference is given to simple and reliable manipulations: puncture of the pleural cavity, laparocenesis, bladder catheterization. Such manipulations take a few minutes of time and are quite reliable in the diagnostic plan. In the case of obtaining air or blood in a pleural cavity or blood in the abdominal cavity, the drainage of the pleural cavity in Büluu or urgent laparotomy is immediately carried out in order to establish a source of bleeding and stopping it. In parallel with the specified operational interventions, osteosynthesis of long bones of the limbs (femoral, tibial, shoulder) and pelvis should be performed. Preference is given to a little traumatic, minimally invasive and short-term methods, primarily osteosynthesis by external fixation devices on a rod basis. Damage to clinically less significant segments (forearm, brush, stop) are fixed with gypsum bandages.
It must be remembered that the goal of emergency operational intervention is a quick stop of bleeding and restoring the function of a damaged organ; Performing various types of plastic, long-term over time and volume of organ-breaching operations is unacceptable. When fixing large bones, the main goal – as soon as possible stable fixation of the fragments; Performing anatomical reposition of fragments is impractical, this is the task of the next phase of assistance.It is enough to eliminate gross displacements in the width and length of the segment.
Traumatic brain injury
If suspected or present traumatic brain injury X-ray examination of the bones of the skull, computed tomography of the brain is mandatory. If it is not possible to perform tomography, then in the presence of clinical data for severe traumatic brain injury and the presence of intracranial hemorrhage, a diagnostic craniotomy is performed, the purpose of which is to revise the epi and subdural spaces, remove the hematomas found and stop bleeding.
Injuries to the chest and abdomen
Such injuries are an indication for urgent surgical interventions. If a hemo- or pneumothorax with rupture of the lungs is detected, drainage of the pleural cavity according to Bulau is urgently performed. If, after removal of the hemothorax, blood continues to flow through the drainage, this indicates continued bleeding. Also informative is the Ruvelua-Gregoire test – if the blood is clotting from the pleural cavity, this indicates ongoing bleeding. With a bleeding rate of more than 200 ml per hour for two hours, as well as with a single release of more than 800 ml of blood, a thoracotomy is indicated.
Rib fractures, especially on both sides, are subject to mandatory anesthesia: local administration of anesthetics, vagosympathetic blockade (on the one hand), catheterization of the subpleural space for periodic administration of anesthetics, alcohol-vocaine blockade.
Slaughter and rupture of the lungs in most cases is accompanied by a contusion of the heart, the diagnosis is made on the basis of ECG data, laboratory and biochemical tests, ultrasound, and the nature of the damage to the chest.
Acute bleeding in the abdominal cavity is an indication for urgent surgical intervention. With simultaneous damage to the organs of the pleural and abdominal cavities, the function of the lungs is first restored, then operations on the internal organs.
Damage to the musculoskeletal system
Conservative treatment of fractures in conditions of multiple and combined injuries not only leads to an increase in unsatisfactory consequences and functional results, but also significantly complicates resuscitation and anti-shock measures and the course of a traumatic disease. At the same time, excessive surgical activity affects mortality rates, and unreasonable conservative tactics worsen the results of social and labor rehabilitation. It must be remembered that intervention on the musculoskeletal system should not be the cause of death.
The purpose and objectives of osteosynthesis at the resuscitation and profile stage are to restore the anatomy and function of damaged segments as soon as possible, to prevent infectious and hypostatic complications.
The main requirements for osteosynthesis of bones in polytrauma are:
• less traumatic and minimally invasive synthesis;
• Possibility of execution by victims in serious condition;
• mobility of victims after osteosynthesis;
• speed and ease of implementation;
• satisfactory immediate and long-term results, absence of reparative disorders;
• Improving the quality of life of victims.
The multiple and combined nature of the injury excludes a stereotyped approach to the choice of osteosynthesis method, and the use of hybrid methods, that is, combinations of osteosynthesis and conservative treatment, is also unacceptable, since in such cases the advantages of osteosynthesis are nullified.
At the resuscitation stage, the choice of osteosynthesis method depends on the general condition of the victim, age and concomitant diseases, type, number, localization and nature of fractures. Fractures of the pelvis and femur are of the greatest importance, and their immobilization by conservative methods (gypsum bandage or skeletal traction) in patients with severe polytrauma is unacceptable.
A modern approach to the treatment of severe traumatic injuries has become the use of the tactics of programmed multi-stage surgical treatment – " damage control surgery ", which is aimed at preventing the adverse development of a traumatic disease by reducing the volume of the first surgical intervention and shifting the final restoration of damaged organs and structures to the stabilization of the vital functions of the body. This means performing a surgical intervention in the minimum necessary volume, for example, stopping the bleeding of a parenchymal organ and its tamponade .
Damage control system in orthopedics (damage control orthopedics) used for fractures of the femur, pelvic bones with damage to the anterior and posterior half rings, multiple fractures of the long bones of the limbs, tearing of the thigh, lower leg. It includes osteosynthesis of the femur, tibia and humerus with external fixation devices; others, as well as injuries in victims of an extremely serious and terminal condition – immobilization with plaster splints or skeletal traction – stage I (within 12 hours from the moment of injury, after performing urgent surgical interventions on the brain, organs of the chest or abdominal cavities). Wounds and open bone fractures are washed with antiseptic solutions, foreign bodies are removed, wound edges are infiltrated with antibiotic solutions, and covered with antiseptic dressings. Simultaneous operations by two or three diversified teams are not allowed. Only the same type of surgical interventions can be performed at the same time, different types of operations are performed sequentially.
In seriously injured patients, operations on the internal organs of the abdomen, small pelvis, chest, brain, which can also be divided into several phases, have priority.
Treatment of unilateral fractures begins with osteosynthesis of the bones of the lower limb, possibly by two teams. Symmetrical fractures – with osteosynthesis of the segment, easier in technical execution. Osteosynthesis of adjacent fractures begins with the distal segment, asymmetric – with a more clinically significant injury. Cross fractures – with osteosynthesis of the bones of the lower limb. In all cases, it is possible to perform osteosynthesis of a more clinically significant segment first.
Stage III – intensive care
Corresponds to II and III periods of traumatic disease. During stage III, against the background of stabilization of vital functions and intensive therapy, delayed surgical interventions are performed to prevent severe complications.
Delayed surgical interventions are called, the failure of which is likely to lead to the development of multiple organ failure and infectious complications. They are performed to the development of complications and is the best way to prevent them.
Such operations include relaparotomy after using tactics damage control surgery (stage II), secondary surgical treatment of wounds (if necessary), patients on mechanical ventilation – tracheotomy.
The meaning of this stage of treatment is intensive therapy aimed at restoring and stabilizing vital functions.
Stage IV – specialized treatment
Corresponds to the IV period of traumatic disease.
During stage IV, the structure and functions of damaged organs and tissues are restored with the help of conservative and surgical measures.
At this stage, the problems of the previous stages of treatment are finally solved, planned surgical interventions are carried out.
Planned – such operations that are carried out according to a previously developed plan to improve the functional results of the account
and creating the most favorable conditions for the consolidation of fractures, the functioning of the joints, wound healing and restoration of the functions of internal organs.
Osteosynthesis of fractures to which the tactics was applied is performed "damage control orthopedics" (stage III), as well as fractures that are fixed with plaster casts with unsatisfactory standing of the fragments, restorative or plastic surgery on internal organs, and the like.