Operation of the Aorticoronary artery shunting (AKSH) Currently, hundreds of thousands of acouter shunt operations were held in the world, and in many clinics they became ordinary. AKSH –
Operation of Aorticorona Shunting (AKSH)
 Currently, hundreds of thousands of Aorticoronary artery shunt operations have been held in the world, and in many clinics they became ordinary.
Currently, hundreds of thousands of Aorticoronary artery shunt operations have been held in the world, and in many clinics they became ordinary.
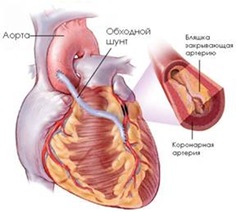
AKSH – Operation aimed at reducing the symptoms of coronary heart disease. The shunt method (eng. Shunt – Bypass) is that with the help of a site of a healthy vein, a bypass path is created for blood flow. This method of treating vascular disease is applied not only in cardiac surgery, but also in the surgery of vessels of other regions.
The pioneer of shunting techniques is considered to be Argentinian Rene Favoro, who first applied this method in the late 1960s. First planned operation AKSH It was completed in the United States at the University of Duke back in 1962 by Dr. Sabista.
There are many differences when it is necessary to prefer the aortocortonary shunting by stenting, but there are indisputable moments when the use of AKS is higher than from stenting:
1. High functional class angina – i.e. Such which does not give the patient to carry out even household loads (walking, toilet, food intake) in the case of anti-steanting contraindications.
2. The defeat of the three and more coronary arteries of the heart (determined during coronaryography).
3. The presence of the aneurysm of the heart against the background of atherosclerosis of the coronary arteries.
Normally, the inner wall of the vessels is smooth and smooth. However, during the development of atherosclerosis on the walls of the vessels, atherosclerotic plaques are formed. They narrow the clearance of blood vessels and disturb the bloodstream in organs and tissues. Over time, the clearance of the vessel is completely closed and the bloodstream stops. This leads in turn to necrosis.
Factors increasing the risk of complications during the operation of the shunting:
1. High blood pressure
2. Obesity
3. Chronic obstructive lung diseases, such as emphysema
4. Renal failure
5. Sugar diabetes
6. Whether the function of the thyroid gland
7. Smoking
Before carrying out aorticon-artistic shunting, as well as all cardiac surgery, a full range of patient survey is carried out, including special research methods such as electrocardiography, coronary art and heart ultrasound.
Operation is carried out only under general anesthesia. Preparation for the operation includes the same events as for other cardiac surgery operations.
The main steps of the operation of the Aorticoronary artery shunting:
- The patient is delivered to the operating room and stacked on the operating table
- Anesthesiologist introduces an intravenous anesthetic to the patient, after which the patient falls asleep
- A special endotracheal tube is inserted into the patient's trachea, through which the patient breathes throughout the operation using a ventilator
- A vertical incision is made in the midline of the chest
- A section of a vein or artery from the indicated places is prepared as a shunt. To create bypass shunts, the veins of the patient's legs are used, as well as the internal thoracic artery,
without these vessels, a person can quite manage. Why are leg veins taken for shunting? The fact is that the veins of the legs are usually relatively "clean", not affected by atherosclerosis. In addition, these veins are longer and larger than other body veins that can be taken.
- The surgeon stops the patient's heart. From this moment on, blood circulation in the patient's body is carried out using a heart-lung machine. It should be noted that in some cases the operation is performed on a beating heart.
- The shunt is sutured with one end to the aorta, and the other to the coronary artery after the narrowing
- The work of the heart is restored
- The chest incision is sutured
- The operation of aortocoronary bypass grafting lasts on average about 3-4 hours. After the operation, the patient is transferred to the intensive care unit, where he stays until the moment of recovery of consciousness – on average, one day. After that, he was transferred to a regular ward of the cardiac surgery department.
- After the operation of arterial bypass surgery, the patient spends in the hospital from 3 to 10 days.
- The sutures from the wound are removed after 7 days.
- The number and length of incisions in the legs may vary from patient to patient, depending on how many vein bypasses you were planning to perform. Someone will have incisions only on one leg, someone on both, someone may have an incision on their arm. First, your stitches will be washed with antiseptic solutions and bandages will be done. Somewhere on the 8th – 9th day, with successful healing, the sutures will be removed, and the safety electrode will also be removed. You may tend to have swelling in your ankles, or you may feel a burning sensation where the veins were taken from. This burning sensation will be felt when you stand or at night. Gradually, with the restoration of blood circulation in the places where the veins were taken, these symptoms will disappear.
In some cases, coronary artery bypass surgery can be performed, as already mentioned above, on a beating heart, without the use of a heart-lung machine. The advantages of this method are:
- no traumatic damage to blood cells
- shorter operation time
- fast postoperative recovery
- no complications associated with the use of cardiopulmonary bypass
Currently, CABG is equally performed both on a beating heart and under cardiopulmonary bypass.When carrying out the operation of aorticoronary artery shunting on a working heart, the risk of operating complications is much lower compared to the operation on the non-working heart, but it is more complex. There is also an opinion that if the AKS is carried out on the working heart, then the quality of the workarounds made from it suffers. That is, according to the remote results, the operation on a working heart can give the worst results compared with the operation on a non-working heart.
Possible complications of aorticoronary shunting:
- Summary infection
- Thrombosis of deep veins
- Insolit or incomplete sobbing sternum
- Complications of anesthesia, for example, malignant hyperthermia
- Myocardial infarction due to reduced pressure, early closure of the lumen of the shunt or damage
- Acute renal failure due to reduced pressure
- Stroke
- The narrowing of the Shunts, especially this concerns the shunt based on Vienna
- The formation of a keloid scar
- Chronic cut pain
- Postoperative complications, in the form of constipation, memory loss, etc.
If the operation of the ACH ends favorably, and this is the overwhelming majority of cases, the patient expects a complex stage of rehabilitation. However, all the inconvenience during this period in several months go to no, and The benefits of the aorticon-artistic shunting in the form of the disappearance of the angina region becomes obvious.
2-3 months after AKS, the Load Dough VEM or Tredmil test is recommended. These tests help determine the condition of imposed shunts and blood circulation in the heart.
Operation ACH is not a panacea and does not guarantee the stops of atherosclerosis and the growth of new plaques in other arteries. Even after the Aorticoronaryth Shunting, all the principles of treatment of ischemic heart disease remain unchanged.
ACHS is carried out only with one goal – to save the patient from angina and reduce the frequency of its hospitalization due to the exacerbation of the process. For all other criteria, such as the risk of re-infarction and the lethal outcome for 5 years – indicators are comparable both in the aorticonial shunting and in stenting or conservative treatment.
For AKS, there are no age limit, it matters only the presence of a concomitant pathology limiting the conduct of a credit operation. In addition, if the operation of the aortocortonary shunting was already carried out earlier, the risk of complications in the event of a re-ACHER is made much higher, and such patients are rarely taken to re-operation.
