Normally, the regular contractions of our heart are supported by special cells that form the sinus node. This structure is located in the top…
Without a keyword
Normally, the regular contractions of our heart are supported by special cells that form the sinus node. This structure is located in the upper part of the right atrium. (Fig. 1)
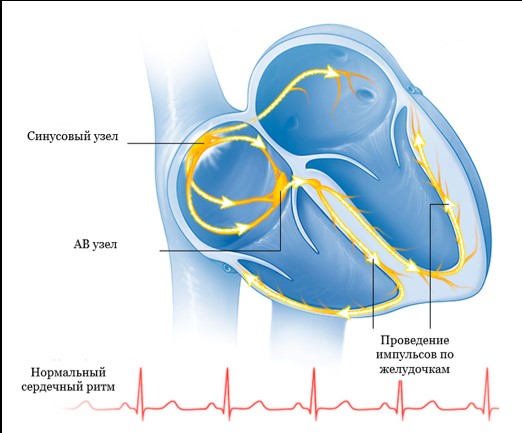
Figure 1 Formation and propagation of electrical impulses in normal
In some cases, the normal functioning of the heart may be disturbed, patients may feel an irregular, fast or slow pulse, pauses between contractions. All this is called a heart rhythm disorder or arrhythmia.
There are several types of arrhythmias:
Supraventricular arrhythmias:
- Fibrillation and atrial flutter
- Supraventricular paroxysmal tachycardia
- Atrial extrasystole
Ventricular arrhythmias:
- Ventricular extrasystole
- Ventricular tachycardia
What is paroxysmal tachycardia?
Under normal conditions, the normal heart rate is between 60 and 100 beats per minute. A heart rate over 100 beats per minute is called tachycardia.
With paroxysmal tachycardia, a sudden attack (paroxysm) of rapid heartbeat occurs, usually without regard to physical activity.
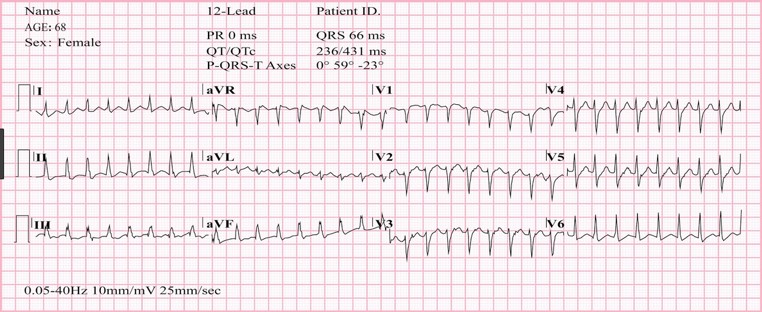
Figure 2 Paroxysm of supraventricular tachycardia with a frequency of 180 per minute.
Paroxysm of tachycardia is a regular heartbeat with a frequency, as a rule, from 150 to 200 beats per minute, which is accompanied by weakness and shortness of breath. (Figure 2) Sometimes patients may lose consciousness. In some patients, these episodes are of short duration and are not accompanied by severe symptoms.
How is extrasystole manifested?
An extrasystole is a premature contraction of the heart, which is felt by patients as a short interruption in the work of the heart, after which there may be a short pause, followed by the restoration of a rhythmic heartbeat.
Treatment of arrhythmias
For the treatment of various types of arrhythmias, both medicinal and surgical methods of treatment are used. Among the surgical methods of treatment, catheter ablation is the most common.
What is ablation?
Catheter ablation is a minimally invasive operation during which the “source” of arrhythmia is eliminated using radio frequency energy (RFA) or local cooling of the heart tissue (cryoablation).
The emergence of the catheter ablation technique was the result of the intensive development of science and the emergence of new medical technologies over the past 20 years.
Today, the method of catheter ablation is widespread throughout the world (more than 1 million operations annually) and is the only treatment method that can radically eliminate a significant part of human heart rhythm disturbances.
Types of catheter ablations
Most often in clinical practice, the current is used super high (radio) frequency – 500 kHz. This type of ablation is called radio frequency catheter ablation (RCH). The effects of radio frequency energy are carried out with the help of special controlled catheters installed in the heart under X-ray control. (Fig. 3)
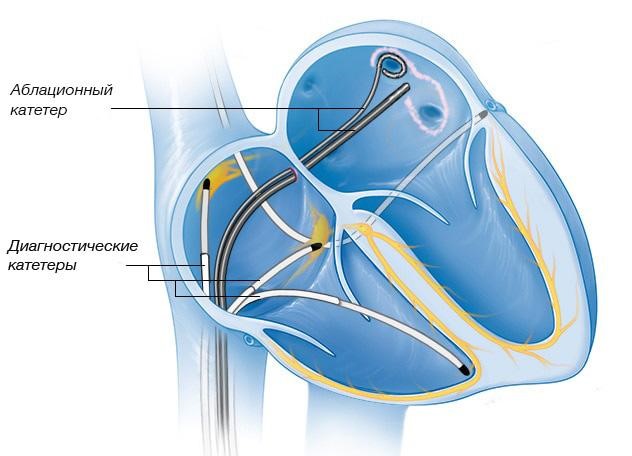
Figure 3 Location of catheters in the heart during RCH.
Another type of exposure to the source of arrhythmia is based on the rapid, deep and local cooling of the tissues of the heart. This type of catheter ablation was called catheter cryoablation. Most often, catheter cryoablation is used to treat atrial fibrillation, for this is used by a special cryobalon catheter. This type of operation is called catheter balloon cryoablation. (Fig. 4)
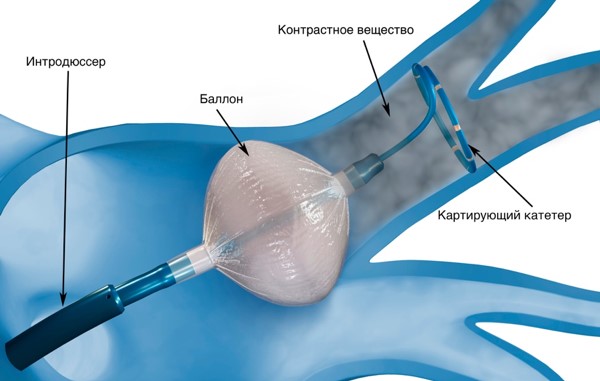
Figure 4 The location of the cylinder in the left atrium during the cryoablation.
What types of arrhythmias can be eliminated with the help of catheter ablation?
All the violations of the rhythm in humans are accepted depending on the localization of the "source" of arrhythmia in the heart of a person on the "supersparce" and "ventricles". The cause (etiology) of the Human arrhythmias can be various pathological effects on the heart (inflammation, ischemia, etc.), or they may be due to congenital features (anomalies) of the development of the heart, incl. Conductive heart system. Often to detect the cause of the development of arrhythmia. Such violations of the rhythm (in the absence of other diseases of the heart) are called "idiopathic". The method of catheter ablation allows in most cases to effectively eliminate various both by etiology and in development mechanisms, arrhythmias.
Advantages of catheter ablation
Treatment of heart rate disorders can be drug or interventional (surgical). It should be borne in mind that drug treatment provides for a long, often lifelong taking antiarrhythmic drugs. The cessation of drug intake or a reduction in the dose creates conditions for recurrence of arrhythmias. In addition, the use of medicines is often impossible due to side effects or contraindicated due to the presence of concomitant heart disease.
Now international and domestic recommendations for the treatment of heart rate disorders consider the method of catheter ablation as the main method of treating a significant part of rhythm violations. Such recommendations are based on the fact that the catheter ablation eliminates the arrhythmia without resorting further to the use of antiarrhythmic drugs.
In accordance with the recommendations, the ablation is recommended in the following cases:
– as the main method of treatment with arrhythmias, where the use of catheter ablation is accompanied by high efficiency and safety (taching tachycardia, atrial trembles)
– as an alternative type of treatment, as a rule, with the ineffectiveness of drug therapy or the development of side effects of antiarrhythmic drugs (atrial fibrillation, ventricular arrhythmias)
About catheter ablation
Before RFA, the department performs the necessary examination (blood tests, instrumental diagnostic methods) within, as a rule, 2-3 days. On the day of the operation, the patient does not eat breakfast; immediately before the operation, he puts on compression stockings (anti-thromboembolic stockings or elastic bandages).

RFA is performed by interventional arrhythmologists in an X-ray operating room equipped with modern equipment for diagnostics and interventional treatment.
As the first stage of the operation, the so-called. intracardiac electrophysiological study (VEFI), the purpose of which is to clarify the type of tachyarrhythmia and search for the source of arrhythmia. (Fig.3 and Fig.4)
To do this, perform a puncture of the vessels (the femoral vein and, if necessary, the artery), under X-ray control, special diagnostic electrodes are carried out. During VEFI, electrical stimulation of the heart of various parts of the heart is performed in accordance with diagnostic algorithms. This allows you to establish an accurate diagnosis and determine the localization of the source of arrhythmia.
In some cases (with atrial fibrillation), inhalation anesthesia is used as an anesthetic aid, in other cases, local anesthesia.
The duration of the operation is determined by its volume and takes from 1.5 to 3 hours.
After RFA, a pressure bandage is applied to the vessel puncture site and the patient is transferred to the postoperative ward, where he is under the supervision of an anesthesiologist-resuscitator for at least 12 hours. All this time the patient is on strict bed rest.

To exclude possible complications after RFA, all patients undergo a comprehensive postoperative examination.
On average, the period of hospitalization for RFA does not exceed 5 days.
Safety and efficiency
The effectiveness of catheter ablation, depending on the type of arrhythmia, ranges from 70 to 99%. The risk of potential complications after surgery, as a rule, does not exceed 1%, but can reach 4-5% for the most complex cardiac arrhythmias. The decision to conduct interventional treatment in each case is made by our specialists, taking into account the opinion of the patient, based on full information about the benefits and potential risks of surgical treatment.
Catheter ablation of atrial fibrillation
What is Atrial Fibrillation?
With atrial fibrillation (atrial fibrillation), instead of a regular heart rhythm, multiple electrical waves occur in the atria, leading to chaotic contractions of both atria with a very high frequency. [Rice. 5]
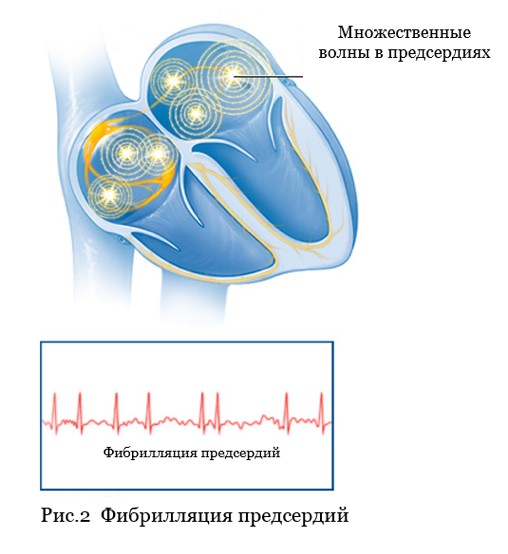
Figure 5. Atrial fibrillation
Atrial fibrillation (atrial fibrillation), as a rule, is manifested by a rapid irregular heart rate, shortness of breath, and poor exercise tolerance. Often, atrial fibrillation is asymptomatic and is detected incidentally during ECG recording.
Often in patients with atrial fibrillation (atrial fibrillation), another type of heart rhythm disturbance is found – atrial flutter. [ Fig.6 ]
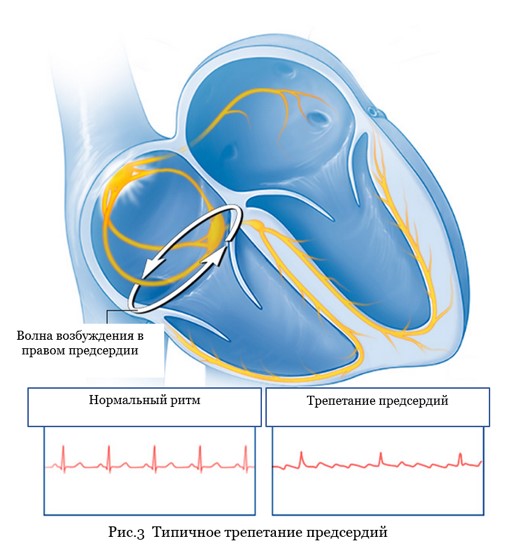
Figure 6. Typical atrial flutter.
Symptoms of atrial flutter differ little from atrial fibrillation. Accurate diagnosis of these rhythm disturbances and treatment tactics should be determined by a cardiologist-arrhythmologist.
Why and how to treat atrial fibrillation?
Treatment of atrial fibrillation aims to: 1) eliminate the symptoms of arrhythmia, i.e. improving the quality of life of patients; 2) elimination of the threat of development of heart failure; 3) prevention of thromboembolic complications.
According to world medical statistics, atrial fibrillation (atrial fibrillation) is the most common (1-2% in the population) heart rhythm disorder. In a significant proportion of patients (up to 40%), AF is asymptomatic. In this category of patients, drug antiarrhythmic or non-drug treatment (catheter ablation) of AF, as a rule, is not performed. The treatment of these patients is to control the heart rate and prescribe anticoagulants to prevent thromboembolic complications.
Patients in whom atrial fibrillation is accompanied by the symptoms described above are prescribed permanent antiarrhythmic therapy aimed at preventing recurrence of AF. Approximately one third of all patients with AF can find an effective antiarrhythmic drug or a combination of them.
In 30% of patients with symptomatic, poorly tolerated atrial fibrillation, it is not possible to choose an effective antiarrhythmic therapy, or taking antiarrhythmic drugs is contraindicated, accompanied by the development of side effects, or patients do not want to adhere to the tactics of long-term conservative drug treatment. This category of patients, in accordance with modern international and Russian recommendations, is indicated for catheter ablation.
It should be emphasized that the choice of treatment options in each case is the task of a cardiologist-arrhythmologist, taking into account the opinion of the patient and objective medical data.
Catheter and surgical ablation
Depending on the form of atrial fibrillation (paroxysmal, persistent or permanent), the presence of other pathologies from the cardiovascular system and concomitant diseases, 3 types of catheter (or surgical) ablation are used:
Intracardiac catheter ablation is the most widely used method of non-pharmacological treatment of AF.Catheter ablation is performed in an X-ray operating room using guided catheters that are moved into the heart chambers through vascular accesses (femoral and subclavian veins). The purpose of the operation is the radical elimination of the “sources” of arrhythmia in the left and (with atrial flutter) right atrium. Currently, 2 types of catheter ablation have found wide clinical use: radiofrequency catheter ablation and balloon cryoablation.
Catheter ablation (destruction) of the AV node is a type of intracardiac catheter ablation, which is used in cases where AF is accompanied by a persistently high heart rate when medical control or radical elimination of AF is impossible. Ablation of the AV node is performed only after the implantation of an artificial pacemaker (pacemaker).
Operation "Labyrinth" – surgical ablation of AF. The maze operation (MAZE) is used in cases where a patient with AF is indicated for open heart surgery due to the presence of an “underlying” heart disease: coronary artery bypass grafting, valve replacement, etc. As an independent intervention in AF, the labyrinth operation is used in the form of modified minimally invasive operations with thoracoscopic access (through a small incision in the chest) and only if previous attempts at catheter ablation have failed.
RFA or cryoablation?
According to modern concepts, the key role in the development of AF belongs to the so-called "arrhythmogenic" pulmonary veins (the so-called AF triggers) – large vessels that flow into the left atrium. [ Fig.7 ]
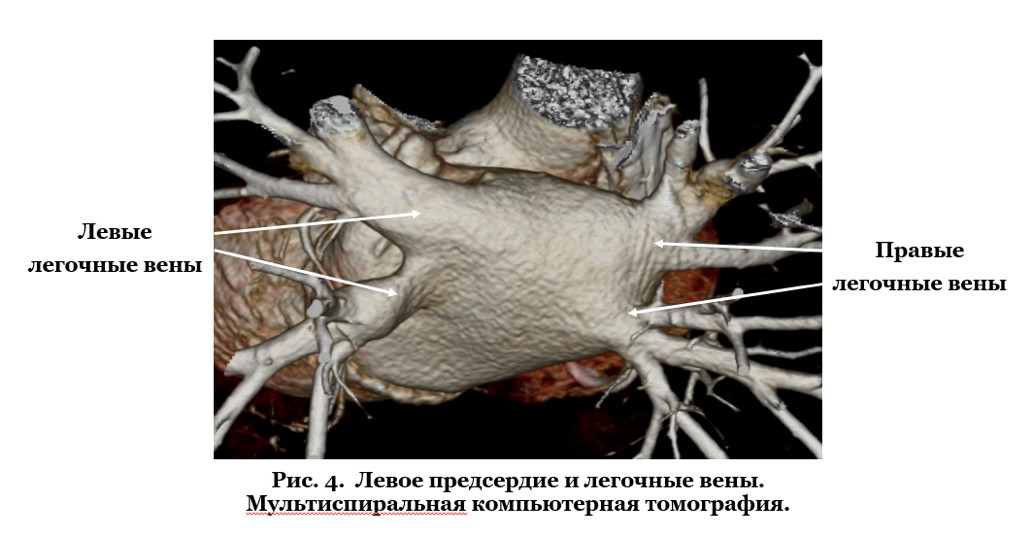
Figure 7. Left atrium and pulmonary veins. Multislice computed tomography
That is why most patients with paroxysmal and persistent forms of atrial fibrillation are shown to perform catheter ablation (isolation) of the pulmonary veins.
How it works?
In radiofrequency catheter ablation, isolation of the pulmonary veins is achieved by applying a large number of point impacts using high frequency current. These exposures should form a continuous chain of many successive coagulation necrosis around each of the veins [Figure 8A]. When using another technology – balloon cryoablation , a necrosis zone around the veins is created due to the effect of low temperature (up to -60ºС) in a cryoballoon located sequentially in each of the pulmonary vein ostia [Fig. 8B].
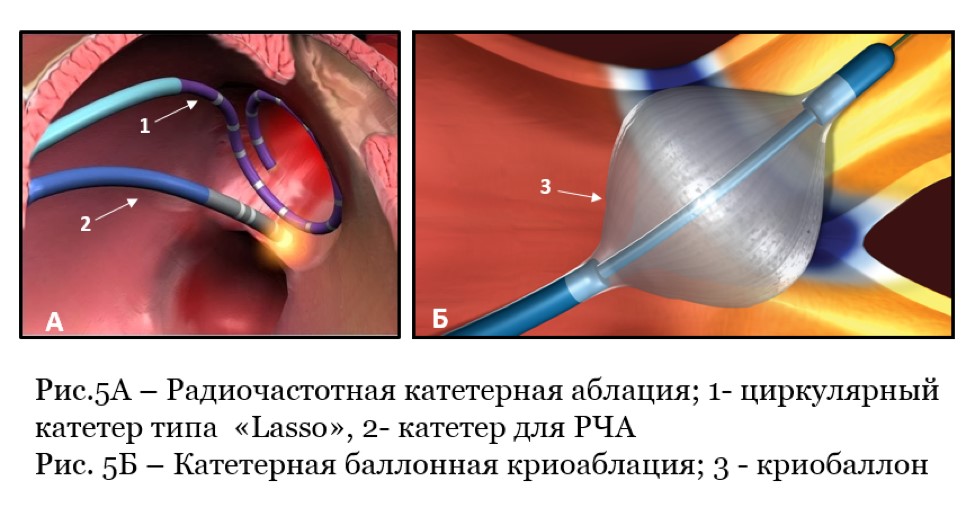
Rice. 8A – Radiofrequency catheter ablation (RFA); 1-circular diagnostic electrode type “Lasso”, 2- catheter for RFA
Rice. 8B – Catheter balloon cryoablation: 3-cryoballoon
Video 1. Balloon cryoablation.
In most cases, complete isolation is achieved by a single cryotherapy for several minutes, which is an absolute advantage over radiofrequency ablation.Both types of catheter ablations are performed in an X-ray operating room under anesthesia or under deep sedation. These interventions are high-tech types of medical care and should be performed by qualified specialists with sufficient experience in interventional interventions.
Efficacy and safety
The generally accepted definition of the effectiveness of catheter ablation in AF is the absence of any atrial arrhythmias after surgery without the use of antiarrhythmic drugs. Efficacy is monitored clinically (patient self-monitoring) or using long-term ECG recording systems (HM ECG or special implantable heart rate recorders).
One of the main factors determining the effectiveness of catheter ablation in AF is the duration of fibrillation episodes. In cases where arrhythmia attacks do not exceed a few hours or days (the so-called paroxysmal form) and, as a rule, are pumped on their own, the operation is most effective. In comparative studies (international study "Fire and Ice"), 65% of patients did not have AF recurrence during the first year, both after RFA and after balloon cryoablation. At the same time, there are observations that in persons without concomitant cardiac pathology, the effectiveness of balloon cryoablation can reach 80-90%.
In patients with persistent AF, i.e. with an arrhythmia lasting more than 7 days, and also requiring medical or electrical cardioversion to restore sinus rhythm, the expected effectiveness of catheter ablation is about 50-60%.
If, after catheter ablation, AF recurs with the same frequency and duration, re-intervention is justified.
Complications in catheter ablation of AF can manifest as vascular damage at the puncture site, perforation of the heart wall with the development of tamponade, thrombus formation in the heart cavity and thromboembolic complications, thermal damage to the esophagus, development of phrenic nerve paresis, and a number of others. The use of modern high-tech control methods during intracardiac interventions, sufficient experience and qualifications of the doctor allows you to perform these interventions effectively and without a significant risk of complications.
At the same time, it is necessary to clearly realize that the decision to conduct interventional treatment of AF should be made by a doctor with sufficient experience in treating such a category of patients, objectively taking into account the pros and cons.
Catheter ablation of AF in the Department of Clinical Electrophysiology and X-ray Surgery of Rhythm Disorders
Interventional arrhythmology has been one of the main directions in the scientific and clinical work of the Department of Clinical Electrophysiology since its foundation in 1990.Almost 20 years of experience in the treatment of various cardiac arrhythmias using catheter ablation technology.
Since 2012, the department has introduced the method of catheter ablation in AF. Today, the priority method used in the clinical practice of the Department of Clinical Electrophysiology for non-pharmacological treatment of AF is the method of balloon cryoablation. This choice is based on the fact that cryoablation in AF is not inferior in effectiveness to radiofrequency, while being the safest method of interventional treatment of AF, which was proven by analyzing many years of experience of the world's leading centers in the treatment of AF.
Specialists of the Department of Clinical Electrophysiology conduct a full preoperative examination of patients, perform interventional intervention and provide outpatient monitoring of all patients for at least 1 year after catheter cryoablation of AF. In cases where patients have complex concomitant cardiac arrhythmias, complex (simultaneous) interventional treatment is used, or the so-called. "hybrid therapy" combining catheter intervention and subsequent drug treatment. If AF recurs, repeat balloon cryoablation or radiofrequency catheter ablation may be performed.
Radiofrequency ablation of paroxysmal supraventricular tachycardias
The most common types of paroxysmal supraventricular tachycardias are:
– Paroxysmal atrioventricular nodal reciprocal tachycardia or AV nodal tachycardia. It is characterized by the presence of a congenital anomaly – an additional path in the AV node, which normally conducts an impulse from the atria to the ventricles. This anomaly is the cause of tachycardia (Fig. 9);
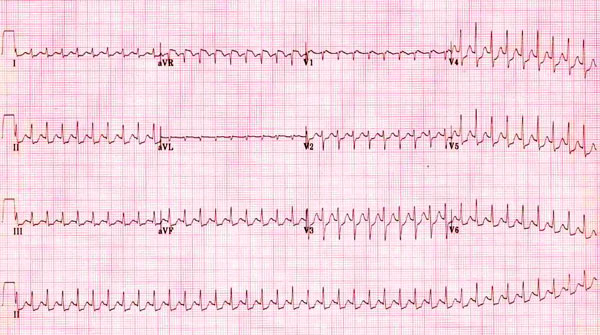
Rice. 9. Paroxysm of AV-nodal tachycardia on the ECG.
– Paroxysmal tachycardia in Wolff-Parkinson-White syndrome (WPW syndrome) also occurs due to a congenital anomaly – an additional path between the atria and ventricles (p. Kent). (Fig. 10);
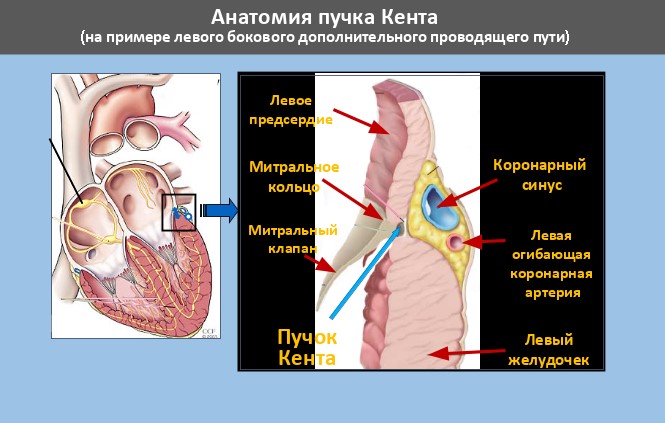
Fig. 10 Kent's bundle of left lateral localization
– Atrial tachycardia can have a source in both the left and right atria (Fig. 11), and may be the result of concomitant heart diseases (ischemic heart disease, hypertension or valvular disease), or have a so-called. idiopathic (without comorbidity) character.
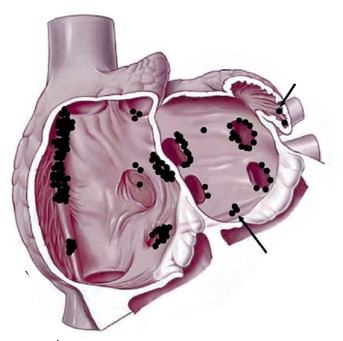
Fig. 11 Sources of atrial tachycardia in the left atrium (indicated by arrows)
An ECG recorded during a paroxysm of tachycardia often does not allow an accurate diagnosis.
It can be clarified by such examination methods as transesophageal pacing (TEPS) or intracardiac electrophysiological examination (VEFI), which are standard methods for diagnosing arrhythmias.
Surgical treatment of the above types of tachycardia using radiofrequency ablation (RFA) allows you to completely get rid of arrhythmia, the effectiveness of the method is 97-99%.At the same time, the risk of potential complications of RFA, as a rule, does not exceed 1%.
Ventricular tachycardia
With ventricular tachycardia, the pathological impulse circulates in the tissues of the myocardium of the right or left ventricles.
This type of arrhythmia can occur in healthy individuals without any serious heart disease. Often, these heart rhythm disturbances are benign and do not always require treatment.
In other cases, ventricular tachycardias may be the result of serious diseases such as myocardial infarction, which can cause sudden cardiac death. (Fig.12)
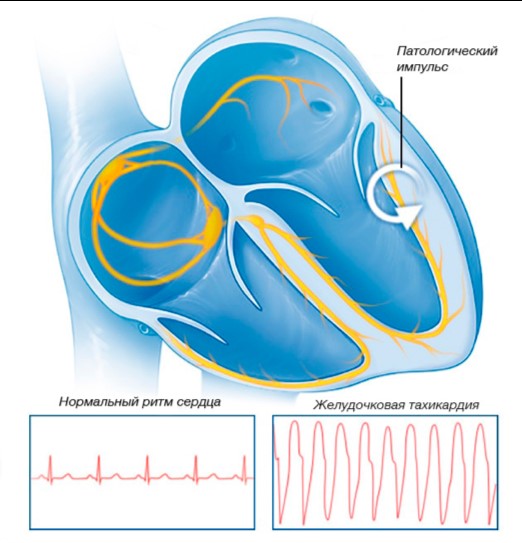
Figure 12 Ventricular tachycardia
Currently, non-drug therapies such as radiofrequency ablation (RFA) or implantation of a cardioverter-defibrillator are commonly used to treat ventricular tachycardias.
To select the optimal method of treatment, a comprehensive examination is necessary.
