The recommendations of the All-Russian Public Organization "Federation of Anesthesiologists and Resuscitations" are devoted to the current state of the problem of using non-invasive ventilation of light and high-flow oxygenation in acute respiratory failure of various genes. Recommendations used a pathophysiological approach to the choice of the respiratory support method, describes the advantages and disadvantages of methods, is given a clinical studies from the standpoint of evidence-based medicine. Based on the presented analysis, recommendations and algorithm on the use of non-invasive artificial ventilation of light and high-flow oxygenation in respiratory failure of various genes indicating the level of evidence and class of recommendations.
Without kewood
VDI – Upper Respiratory Ways
VPO – high strength (high-speed) oxygen therapy
DN – respiratory failure
Up – respiratory volume
ZSN – stagnant heart failure
IVL – artificial lung ventilation
Nivl – non-invasive lung ventilation
NP – Nosocomial Pneumonia
Odn – acute respiratory failure
ORDS – acute respiratory distress syndrome
Orit – Department of Resuscitation and Intensive Therapy
OSN – acute heart failure
RP – Respiratory Support
COPD – chronic obstructive pulmonary disease
CH – respiratory frequency
CPAP (Continuous Positive Airway Pressure) – Continuous Positive Pressure Pressure
EPAP (EXPIRATORY POSITIVE AIRWAY PRESSURE) – Pressure pressure on exhalation
FIO.2 – fraction of oxygen in the inhaled gas emission
IPAP (Inspiratory Positive Airway Pressure) – Inspiratory Pressure
PAO.2 – partial oxygen pressure in arterial blood
PAO.2/ FIO.2 – Oxygenation index
Paco.2 – Partial carbon dioxide pressure in arterial blood
PEEP (POSITIVE END-EXPIRATORY PRESSURE) – positive outflow end pressure (positive final expiratory pressure)
PS (Pressure Support) – the magnitude of the support of inspiratory pressure
PSV (Pressure Support Ventilation) – Ventilation with support for inspiratory pressure
SRO2 – Saturation of hemoglobin oxygen (according to the pulse oximeter)
Terms and Definitions
Respiratory failure – The condition of the body, in which the normal gas composition of arterial blood does not ensure, or it is achieved due to the increased operation of the external respiratory, leading to a decrease in the functionality of the body, or is supported by artificially.
Acute respiratory failure – This is the inability of the respiratory system to ensure the flow of oxygen and the removal of carbon dioxide necessary to maintain the normal functioning of the body.
1. Brief information
1.1.Definition
Non-invasive lung ventilation (NIVL) It is an option for respiratory support without endotracheal access (through nasal or facial masks, helmets) using all known auxiliary ventilation modes. In a number of clinical situations, Nivl has undeniable advantages over traditional artificial pulp ventilation (IVL), since it leads to a decrease in the frequency of nosocomial infections, complications and mortality [1-5].
1.2. Epidemiology
In modern resuscitation and intensive therapy, one of the most pressing problems is severe acute respiratory failure (ODN), which requires prosthetics of the function of external respiration. According to various estimates, in the United States registered up to 137 cases of severe one per 100,000 population, 31-day mortality is 31.4% [1]. In Europe, the prevalence of severe one is from 77.6 to 88.6 cases per 100,000 population per year, for acute respiratory distress syndrome (ORDS) these figures range from 12-28 cases per 100,000 population per year. In Russia, according to various data, on average, 15,000 ODU cases are registered, with a more frequent development of severe one in the resuscitation separation, depending on the nature of diseases, damage and injuries (on average from 18 to 56% of all patients in OR). The frequency of use of Nivl in Russia is no more than 1% [5].
Currently, artificial ventilation of the lungs (IVL) remains the main type of assistance in the branches of the anesthesiology-resuscitation [2]. It is evidence that 33% of patients received in the ward of intensive therapy are required at least 12 hours. Indications for IVL: one (69% of cases), coma (16%), respiratory failure in chronic lung diseases (13%) , neuromuscular diseases (2%) [2, 3]. The duration of the IVL averages 5 days, however, 1% of Ivl patients apply more than 28 days. Consolidated data on the frequency of NVL is missing.
1.3. Coding on the ICD-10
J12 – viral pneumonia, not classified in other categories.
J13 – Pneumonia caused by Streptococcus pneumoniae.
J17 – Pneumonia in diseases classified in other categories.
J18 – Pneumonia without refining the causative agent.
J46 – Astmatic status [Status AsthMaticus.].
J80 – respiratory disorder syndrome [Disteres] in an adult.
J81 – pulmonary edema.
J96 – respiratory failure, not classified in other categories.
1.4. Coding on the nomenclature of medical services
Coding on the nomenclature of medical services According to the order of the Ministry of Health of the Russian Federation of October 13, 2017 No. 804n "On Approval of the Nomenclature of Medical Services" (with changes and additions):
1.5. The main advantages and disadvantages of non-invasive respiratory support
Nein invasive respiratory support include NIVL itself (through masks or helmets), as well as high-flow oxygenation carried out through special nasal cannulas.
Nivl (compared to invasive IVL, carried out through the endotracheal tube, and standard hydrocerapy) has a number of advantages and disadvantages.
Advantages of NivlDefinition
Non-invasive lung ventilation (NIVL)
It is an option for respiratory support without endotracheal access (through nasal or facial masks, helmets) using all known auxiliary ventilation modes. In a number of clinical situations, Nivl has undeniable advantages over traditional artificial pulp ventilation (IVL), since it leads to a decrease in the frequency of nosocomial infections, complications and mortality [1-5].
1.2. Epidemiology
In modern resuscitation and intensive therapy, one of the most pressing problems is severe acute respiratory failure (ODN), which requires prosthetics of the function of external respiration. According to various estimates, in the United States registered up to 137 cases of severe one per 100,000 population, 31-day mortality is 31.4% [1]. In Europe, the prevalence of severe one is from 77.6 to 88.6 cases per 100,000 population per year, for acute respiratory distress syndrome (ORDS) these figures range from 12-28 cases per 100,000 population per year. In Russia, according to various data, on average, 15,000 ODU cases are registered, with a more frequent development of severe one in the resuscitation separation, depending on the nature of diseases, damage and injuries (on average from 18 to 56% of all patients in OR). The frequency of use of Nivl in Russia is no more than 1% [5].
Currently, artificial ventilation of the lungs (IVL) remains the main type of assistance in the branches of the anesthesiology-resuscitation [2]. It is evidence that 33% of patients received in the ward of intensive therapy are required at least 12 hours. Indications for IVL: one (69% of cases), coma (16%), respiratory failure in chronic lung diseases (13%) , neuromuscular diseases (2%) [2, 3]. The duration of the IVL averages 5 days, however, 1% of Ivl patients apply more than 28 days. Consolidated data on the frequency of NVL is missing.
1.3. Coding on the ICD-10
J12 – viral pneumonia, not classified in other categories.J13 – Pneumonia caused by
Streptococcus pneumoniae.
J17 – Pneumonia in diseases classified in other categories.
J18 – Pneumonia without refining the causative agent.
J46 – Astmatic status [
Status AsthMaticus.
J80 – respiratory disorder syndrome [Disteres] in an adult.
J81 – pulmonary edema.
J96 – respiratory failure, not classified in other categories.
1.4. Coding on the nomenclature of medical services
Coding on the nomenclature of medical services According to the order of the Ministry of Health of the Russian Federation of October 13, 2017 No. 804n "On Approval of the Nomenclature of Medical Services" (with changes and additions):
1.5. The main advantages and disadvantages of non-invasive respiratory support
Nein invasive respiratory support include NIVL itself (through masks or helmets), as well as high-flow oxygenation carried out through special nasal cannulas.
Nivl (compared to invasive IVL, carried out through the endotracheal tube, and standard hydrocerapy) has a number of advantages and disadvantages.
Advantages of Nivl Before invasive IVL as follows:
1) the lack of complications from the intubation of the trachea and the long-lasting endotracheal tube;
2) reducing the frequency of nosocomial infections;
3) a decrease in the need for medication sedation;
4) the non-invasive nature of the procedure and its simplicity;
5) the possibility of earlier patient mobilization;
6) Economic efficiency.Advantages of Nivl
Before standard hydrocerapy through the facial mask or nasal cannulas are as follows:
1) ensuring a positive finite-expiratory pressure (PEEP) or constant positive pressure in the respiratory tract (CPAP);
2) providing inspiratory pressure (PINSP or inspiratory positive pressure in the respiratory tract – iPap) with adjustment of the trigger inhalation and exhalation;
3) adequate moisturizing and heating of the respiratory mixture.Nivl flaws:1) the need for active cooperation of the patient with medical personnel; 2) the inability to apply a high level of inspiratory and expiratory pressure;
3) lack of direct access to respiratory tract for rehabilitation;4) high risk of aerophagia;
5) the high risk of aspiration of the content of the oral cavity and the stomach;
6) Mazrasion and skin necrosis in places of adjustment;
7) hypoxemia when displaced mask;9) drying and nasopharynx;
10) Nasal bleeding.Recommendation 1.
Based on the pathophysiology of the DN and NIVL technology, its advantages are implemented in the following situations:
1. Expuratory closure of small respiratory tract, chronic obstructive pulmonary disease (COPD) – the patient requires oxygen therapy in combination with a moderate level of reer / crash to facilitate expiratory flow and a moderate level of inspiratory pressure for unloading respiratory muscles (level of evidence of evidence – 1, the level of persuasiveness of recommendations – BUT).
2. Hypoxcemic (parenchymal) OND with low potential of recubibilities of alveoli (pneumonia, lung injury, pulmonary artery thromboembolism (TEL) with the development of infarction pneumonia,The state after resection of the lung) – the patient needs oxygen therapy in combination with a low level of reer / sterry and low levels of inspiratory pressure (iPap, PS) to unload the respiratory muscles (the level of evidence of evidence – 2, the level of persuasiveness of recommendations – c).
3. Hypoxmic OND with a low potential of recubibilities of the alveoli in combination with immunosuppression (pneumatic pneumonia, one in oncohematology, ODN after transplantation of solid organs) – the patient needs oxygen therapy in combination with a moderate level of reer / crash and a moderate level of inspiratory pressure for unloading respiratory muscles (level Evidence of evidence – 2, the level of persuasive recommendations – c).4. Acute left vehicle failure and cardiogenic pulmonary edema – the patient needs oxygen therapy in combination with a moderate reur / crash level to reduce the impact work of the left ventricle and moderate inspiratory pressure for unloading the respiratory muscles (the level of evidence of evidence – 1, the level of persuasiveness of recommendations – a).5. Prevention of postoperative atelectasis in patients of high-risk groups (obesity, immunosuppression, COPD with hypercapnia, thoracic surgical interventions) – the patient's need for a moderate level Reer / Crypt for the prevention of atelectasis (the level of evidence of evidence – 2, the level of persuasiveness of recommendations – c).
Comments *.
Nivl does not violate the natural mechanisms of anti-infectious protection, which causes its advantages over invasive IVL in patients with the development of OND with immunosuppression, including at the exacerbation of COPDs against the background of adhesion of glucocorticosteroids, and in acute left vehicles, which is often developing in elderly patients with weakened immunity. [4].
Nivl provides an adequate specified oxygen level in combination with a moderate level of reer / CPAP and inspiratory pressure,что обусловливает преимущества перед стандартной оксигенотерапией через лицевую маску или носовые канюли у пациентов с ограничением экспираторного потока вследствие экспираторного закрытия мелких дыхательных путей (ХОБЛ), так как облегчает экспираторный поток, уменьшая работу дыхания и снижая собственный уровень (ауто)РЕЕР, а также разгружая дыхательные мышцы [6].
НИВЛ обеспечивает адекватный заданный уровень кислорода в сочетании с умеренным уровнем РЕЕР/CPAP и инспираторного давления, что обусловливает преимущества перед стандартной оксигенотерапией через лицевую маску или носовые канюли у пациентов с гипоксемической (паренхиматозной) ОДН при невысокой рекрутабельности альвеол (пневмония, ателектазы), когда нужен умеренный уровень РЕЕР и инспираторного давления для предотвращения коллапса альвеол и ателектазирования.
НИВЛ обеспечивает умеренный уровень РЕЕР/CPAP, который снижает пред- и постнагрузку левого желудочка, уменьшая ударную работу левого желудочка, что имеет преимущества перед стандартной оксигенотерапией через лицевую маску или носовые канюли у пациентов с острой левожелудочковой недостаточностью и/или отеком легких.
Рекомендация 2.
Условиями применимости НИВЛ являются сохранность сознания, возможности сотрудничать с персоналом, отсутствие клаустрофобии (при применении шлемов) —и функционирование всего механизма откашливания мокроты (уровень достоверности доказательств — 3, уровень убедительности рекомендаций — C). — Comments.
При нарушении сознания при НИВЛ высока вероятность аспирации желудочного содержимого и раздувания желудка. При нарушении откашливания мокроты (например, при парезе голосовых связок) и бронхорее необходима частая санация трахеи, что невозможно при применении НИВЛ [6]. Для реализации преимуществ НИВЛ и улучшения исходов необходимо длительное постоянное ношение маски (шлема), что в условиях нарушения сознания (например, при делирии) и отказе сотрудничать с персоналом невозможно [7].Before the beginning of the Nivl, in a preliminary conversation, the patient should clarify the principle of operation of the IVL apparatus, features of mask ventilation, the need for a patient's cooperation with personnel, the importance of understanding the meaning and objectives of the procedure.
In addition, the effectiveness of NIVL influence the structural and functional features of the upper respiratory tract (VDP).
Recommendation 3.2 The use of NIVL is most effective to prevent tracheal intubation with compensated OND in patients of risk groups: exacerbation of COPD, community-hospital pneumonia, pneumonia in immunosuppression, ZSN, cardiogenic pulmonary edema.
Comments * *. The main part of the research on the use of Nivl is devoted to the prevention of intubation in patients of high-risk groups: the exacerbation of the COPD (with compensated ODN) (the level of reliability of evidence – a); Cardiogenic pulmonary edema (level of reliability of evidence – a); community-acquired pneumonia in patients with COPD (level of reliability of evidence – c); Hypoventation syndrome during obesity (the level of reliability of evidence is C).Proof of the level obtained, but to reduce the mortality and the number of complications in the early use of Nivl in these patients. Conducting Nivl is possible not only in the conditions of separation of intensive therapy, but also in the wards of a common profile and at home. 2. Basic testimony and contraindications for non-invasive respiratory support
2.1. Indications for the use of NivlRecommendation 4.
The use of Nivl leads to an improvement in gas exchange, reducing the operation of respiration and improving the forecast compared to oxygen and therapy (through the facial mAso or cannula) for the following states:.
– exacerbation of the COPD (with the development of moderate respiratory acidosis (7.35> pH> 7.25) and compensated ODN) (the level of reliability of evidence – 1, the level of persuasiveness of recommendations – a);– community-acquired pneumonia in patients with COPD (the level of reliability of evidence – 2, the level of persuasiveness of recommendations – c);– cardiogenic pulmonary swelling (level of reliability of evidence – 1, the level of persuasiveness of recommendations – a);– hypoxmic OND in immunocomplete patients (the level of evidence of evidence – 2, the level of persuasiveness of recommendations – c);
– preventing post-speaking one in patients with hypercaps on the background of a COPD or obesity (the level of evidence of evidence – 2, the level of persuasive recommendations – c);– hypoventation syndrome in obesity (the level of reliability of evidence – 2, the level of persuasiveness of recommendations – c).Recommendation 5. Criterion for the choice of NIVL when exacerbating COPD is the presence of respiratory acidosis, and not a level of hypercaps: in the absence of respiratory acid acidosis Nivl has no advantages over standard hydroatherapy, at pH 7.257.35 NIVL should be used to prevent trachea intubation, and at a pH of less than 7.20 As an alternative to IVL (the level of evidence of evidence – 1, the level of persuasive recommendations – a)., Comments.) Randomized controlled studies [8-11] did not show a decrease in mortality and frequency of trachea intubation when using Nivl compared with standard hydrocerapy when exacerbating COPD in the absence of respiratory acidosis, but in these studies there was a decrease in the degree of the disposal.2The most clinically significant results were obtained in patients with exacerbation of COPD and pH 7.25-7.35 – an increase in pH and / or a reduction in respiratory rate, a decrease in the degree of dance [12, 13], which occurs in respondents 1-4 hours after the start of Nivl , as well as a decrease in infectious and noncommunicable complications [14, 15].2 In the results of randomized studies of the comparative assessment of NIVL with invasive IVL in patients with exacerbation of COPD and middle pH 7,20, it is noted that, despite the faster increase in pH and reduce the partial pressure of carbon dioxide in arterial blood (PACO
) In a group of invasive IVL, responders have decreased the duration of the IVL and the duration of treatment in the orort, the frequency of infectious complications, as well as the frequency of repeated hospitalizations during the next year without decreasing mortality [16-18].Recommendation 6.2 With severe exacerbation of bronchial asthma Nivl Malvozmenm, sufficiently drug therapy in combination with2 oxygen therapy, under the progression of one (life-focused asthma) –
Only invasive IVL, Nivl is contraindicated (the level of reliability of evidence – 3, the level of persuasive recommendations – c).
Comments.
With the life-focusing exacerbal asthma ("Near-Fatal Asthma"), which is characterized by the occurrence of the zones of "silent" light with auscultation, the peak stream on exhalation is less than 33% of the maximum [19], the broncho structure is so strong, which leads to the procepted load on the breathing muscles ; This level of load makes it impossible to use not only Nivl, but also invasive IVL in fully auxiliary modes. Due to the low frequency of the development of a serious degree of exacerbation of bronchial asthma, in which hospitalization is necessary in the Nort, controlled studies have not been carried out. With a mild and moderate degree of bronchorate (peak flow on exhalation of more than 50% of the maximum for the patient), the clinical effect of the use of bronchodiators is more pronounced. The metaanalysis of uncontrolled studies did not show the improvement of state in patients from the use of Nivl compared with standard therapy [20]. Nevertheless, a group of patients who have a positive clinical and physiological effect on the use of Nivl [21] was revealed in a retrospective study. This study describes three types of aggravation of bronchial asthma: with severe aggravation of asthma, all patients are intubled; With a slight exacerbation, most patients had sufficiently drug therapy; And only some patients with compensated DN, poorly responding to drug therapy, noted the clinical improvement as a result of the use of Nivl.
Recommendation 7. With a cardiogenic edema of the lungs, NIVL should be applied, as this leads to acceleration of the permission of the edema of the lungs, the improvement of gas exchange, a decrease in respiratory operation and, possibly, a decrease in mortality; The advantages of using any Nivl regime before CPAP (the level of evidence is the level of persuasiveness of recommendations – a); Comments.
НИВЛ при кардиогенном отеке легких уменьшает постнагрузку и преднагрузку левого желудочка, снижая индекс ударной работы левого желудочка, уменьшает работу дыхания пациента и улучшает газообмен [22—24]. С 80-х годов ХХ века опубликовано более 30 исследований об использовании НИВЛ при кардиогенном отеке легких, большая часть которых были одноцентровыми с малой выборкой пациентов. Продемонстрировано улучшение оксигенации, снижение степени гиперкапнии и более быстрое разрешение отека легких при применении НИВЛ по сравнению с оксигенотерапией [25]. В нескольких исследованиях отмечено снижение частоты интубации трахеи при применении НИВЛ по сравнению с оксигенотерапией при кардиогенном отеке легких. Несколько мультицентровых рандомизированных исследований подтвердили эти данные. Самое крупное мультицентровое рандомизированное контролируемое исследование (N.2=1069), проведенное в 26 отделениях экстренной помощи, продемонстрировало улучшение клинико-физиологических параметров в группах CPAP и CPAP + Pressure support (PS) по сравнению с оксигенотерапией, но отсутствие снижения частоты интубации трахеи [26]. В рандомизированном исследовании при сравнении стандартной оксигенотерапии, CPAP и CPAP + PS отмечено улучшение клинико-физиологических параметров, снижение частоты интубации трахеи и снижение 15-суточной летальности при применении НИВЛ в любом режиме по сравнению с оксигенотерапией [27]. В мультицентровом рандомизированном исследовании показано ускорение купирования отека легких при применении CPAP + PS по сравнению с CPAP, но без различий по исходам [28]. Исследователи на основании метаанализов и систематических обзоров всех проведенных исследований [29—37] пришли к следующим выводам: 1. НИВЛ снижает частоту интубации трахеи. 2. НИВЛ уменьшает работу дыхания и ускоряет купирование отека легких. 3. НИВЛ и СРАР вызывают сходные физиологические эффекты, однако НИВЛ с заданным уровнем IPAP имеет преимущества у пациентов с гиперкапнией. 4. НИВЛ не увеличивает частоту развития инфаркта миокарда.2Рекомендация 8.2 При ги
поксемической (паренхиматозной) ОДН НИВЛ показана пациентам в случаях сочетания низкой рекрутабельности альвеол с незначительно сниженной или нормальной податливостью легких и грудной стенки (первичная патология паренхимы легких) как терапия первой линии, особенно у пациентов с иммуносупрессией; этим пациентам обычно требуются невысокие уровни РЕЕР и инспираторного давления (PinspIPAP или PS в сочетании с увеличением инспираторной фракции кислорода. Возможно, высокопоточная оксигенация имеет преимущество у этой категории пациентов. К таким состояниям относят: внебольничную пневмонию при исходном индексе PaO.
/ FIO.более 150 мм рт.ст. (уровень достоверности доказательств — 1, уровень убедительности рекомендаций — A), ушиб легких без нарушения каркасности грудной клетки (уровень достоверности доказательств — 2, уровень убедительности рекомендаций — В), синдром гиповентиляции при ожирении, ОДН после резекции легкого (уровень достоверности доказательств — 2, уровень убедительности рекомендаций — А).
Комментарии.
В когортных исследованиях и метаанализе исследований продемонстрирован положительный эффект от применения НИВЛ как терапии первой линии при гипоксемии у пациентов с внебольничной пневмонией и индексом оксигенации (PaO
/ FIO.
) более 150 мм рт.ст., однако неудача такой терапии с задержкой интубации трахеи и начала ИВЛ приводила к увеличению летальности, положительный эффект был особенно выражен при иммуносупрессии и у пациентов с хронической сердечной недостаточностью [38—43].В мультицентровом рандомизированном исследовании, включившем пациентов с первичной патологией легких (внебольничная пневмония более чем у 60% пациентов), продемонстрировано снижение частоты интубации трахеи и летальности при применении высокопоточной оксигенации по сравнению со стандартной оксигенотерапией и НИВЛ [44].
В 3 рандомизированных исследованиях получены данные о снижении частоты интубации трахеи, уменьшении частоты нозокомиальной пневмонии (НП) при применении НИВЛ по сравнению со стандартной оксигенотерапией при ушибе легких [45—47].In a randomized controlled study, when comparing NIVL and standard hydrochiotherapy in patients with hypoxhemia, after resection of the lung, a decrease in the frequency of intubation of tracheas and mortality in the Nivl group was obtained [48].
Recommendation 9.
It is possible to use Nivl with ORDs easy and moderate degree as therapy of the first line (the level of reliability of evidence – 2, the level of persuasiveness of recommendations – a)The delay in the intubation of the trachea in the ineffectiveness of NIVL with the ORDS leads to an increase in mortality.
Comments.
The method allows you to avoid trachea intubation in some patients with light and moderate ORDS, the successful use of NIVL under the ORDS leads to a sharp decrease in the frequency of NP and mortality [49-51]. The assessment of the clinical ineffectiveness of NIVL under the ORDS is carried out after 1 h: with a decrease in the PAO indicator
/ FIO. less than 175 mm Hg, desynchronization with respirator, respiratory rate increase (CH) above 25-30 respiratory movements per minute, increasing PACO
The occurrence of acidosis shows the intubation of the trachea, invasive IVL [49].Recommendation 10. Nivl and high strength oxygenation in patients with gi
Potsemic (parenchymal) ODN with immunosuppression (oncohematology, pneumatic pneumonia, state after
t Organ Range) Reduces intubation frequency
trachea, np and mortality (level of reliability of evidence – 2, level of persuasive recommendations – a)
Comments.
According to a 5-year-old multicenter observational study of the use of Nivl in oncohmetology, a decrease in mortality was obtained in the case of the use of Nivl as therapy of the first line compared to oxygen inhalation [52]. In the development of hypoxmic OND in the patients of oncomematology, the use of NIVL through a helmet in the CPar mode in the profile compartment led to a decrease in hospitalizations to the orit, a decrease in the frequency of tracheal intubation and mortality [53].
In a multicenter randomized study, when comparing hydrochiotherapy with NIVL in patients, there are no significant differences in the frequency of intubation of tracheas and mortality, however, in this study, a high-strength oxygenation was used in this study [54].POST HOC-analysis of this study demonstrated the advantages of highly flow oxygenation in front of standard hydrocerapy and, possibly, the NIVL to reduce the frequency of tracheal intubation and mortality [55].
In a study type, case-control in patients with pneumatic pneumonia due to the enzyme-acquired syndrome (HIV infection), the use of NIVL compared with the invasive IVL led to a decrease in the frequency of tracheal intubation and mortality [56].
The use of NIVL compared to hydrotherapy in patients after the transplantation of solid organs (liver, kidney, lungs) led to a decrease in the frequency of trachea intubation, sepsis and mortality in the orort [57].
Recommendation 11.
Nivl is shown to prevent the development of post-assubation ODN after surgical interventions in risk patients (COPD with hypercapnia, obesity with hypercapper, ZN); The use of NIVL in patients of these groups with the already developed post-speaking one ineffectively and can lead to a delay in the trachea intubation and deterioration of the forecast (the level of evidence of evidence – 2, the level of persuasiveness of recommendations – a).
Comments. Multicenter randomized study of a comparative assessment of the effectiveness of NIVL and standard hydroatherapy with a developed hypoxmic postoperative ODN after 48 hours and more after the planned tracheal extretion demonstrated a delay to the trachea intubation and an increase in mortality in the Nivl group [58]. In another randomized study of a comparative assessment of the effectiveness of Nivl and standard hydroatherapy with the developed hypoxmic postoperative OND in patients with concomitant chronic heart failure and COPD, differences in the frequency of reintubation and mortality were not obtained [59]. In several randomized studies, a decrease in the frequency of the flowback of the trachea, the mortality in the or 90-day mortality in the prevention of the development of post-speaking one in high-risk patients has been demonstrated (COPD with hypercapnia, ZSN, obesity with hypercapper) [60-63].
2.2.Contraindications for the use of NivlRecommendation 12.
Contraindications for the use of Nivl (the level of reliability of evidence – 3, the level of persuasive recommendations – c).
Non-invasive respiratory support should not be applied in the following cases:
1) lack of self-breathing (apnea);
2) unstable hemodynamics (hypotension, ischemia or myocardial infarction, life-degrading arrhythmia, uncontrolled arterial gi
Persongenia);
3) the inability to ensure the protection of the respiratory tract (cough violation and ch
Otania) and high risk of aspiration;
4) excess bronchial secretion;
5) signs of violation of consciousness (initiation or oppression of consciousness), patient's inability
to cooperation with medical personnel;
6) facial injury, burns, anatomical disorders that prevent mask installation;
7) pronounced obesity;
8) the inability of the patient to remove the mask from the person in case of vomiting;29) active bleeding from the gastrointestinal tract;2) 88—95%.
10) the obstruction of the VDP;
11) mask discomfort;212) Operations on an END.23. Methods of carrying non-invasive respiratory support
Recommendation 13.
It is recommended when conducting the Nivl to use specialized devices for NIVL or IVL devices in Nivl mode, which compensate for leaks and use specialized facial / nasal masks or helmets (the level of evidence of evidence – 4, the level of persuasiveness of recommendations is C).
Comments.
For Nivl, it is preferable to use Specialized IVL devices, adapted to compensate for leaks from under mask, but Nivl can be successfully carried out by any of the existing modern fans that can operate in Nivl mode. In the best way, the systems (fans) used to deliver an air mixture are non-versal contour, as it significantly reduces the "dead" space and facilitates the patient's exhalation, which is carried out in the environment, and not back to the respiratory circuit.To work with a non-obverse circuit, the requirements for the IVL apparatus are even more tightened, and here the devices equipped with a high-performance turbocharger (about 200 l / min or more) are published to the fore (about 200 l / min or more) to compensate for very large leaks (up to 80 l / min).The correct selection of the Nivl regime for each patient is very important, as well as the type of mask (facial or nose) and its size, since patients with high nasal resistance (including in VDI infections) may be less sensitive to nasal ventilation.
For non-invasive respiratory support, nasal masks can be used, oral ("ruined") or facial (orosal) masks, as well as helmets. The choice of mask type is very important. In some types of DN, the type of mask affects the results of the use of Nivl even more than ventilation mode. Compared to the nasal mask, the facial mask is easier to choose in size, and its use is associated with smaller air leaks. However, claustrophobia, cough or vomiting can complicate the use of the face mask. The nasal mask, unlike the facial, does not violate the speech and swallowing, it is better tolerated, has a smaller "dead" space (100 ml) compared to the facial mask (about 200 ml). In addition, when it is used, the risk of inflating the stomach is reduced, since, with nasal ventilation, the lips perform the role of the safety valve during the increase in pressure in the respiratory circuit. Since patients with a heavy dynode, as a rule, breathe through the mouth, at the initial stage it is recommended to use a facial mask. Nasal ventilation can be a reserve method for those patients who have ONN are less pronounced. It is possible to use a combination of facial and nasal masks in the following combination: nasal – during the daytime, facial – at night.The mask must be comfortable and without excessive leaks. The correct selection of the sized mask is very important. Sometimes special belts are used to fix the chin.In the circuit there may be a moisturizer, but the heater should be turned off, since the function of the VDP with non-invasive ventilation is preserved.
The mask, as a rule, makes it possible to maintain a rather high level of Croar – up to 15 cm Water.st., but higher levels of pressure (> 18 cm water)) With a non-invasive technique, the crash is difficult because of the leaks from the mask.
The type and properties of the trigger used to provide an auxiliary ventilation, namely, play an important role. The smaller the delay time, the faster the support of the efforts of the respiratory muscles on the breath and the better the synchronization of the patient and the respirator. It is desirable that the "response" of the respirator on the inspiratory attempt of the patient began not later than 0.05-0.1 s, otherwise the patient will have to perform additional work during the inhalation to overcome the resistance of the contour of the device.
There are data on the best tolerability by patients, greater efficiency of NIVL and fewer complications when using special helmets for NIVL compared to mask ventilation of the lungs [64, 65].
Recommendation 14.
When conducting Nivl, it is recommended to start with a standard technique (see Appendix B) (the level of reliability of evidence – 3, the level of persuasive recommendations – c).2For non-invasive respiratory support traditionally used the reer mode (CPAP, EPAP) with a pressure level from 5 to 10-12 cm water. Either his combination with the support of inspiratory pressure (PSV) – (iPap). Currently, Nivl modes are practically no different from the invasive IVL (CPAP, CPAP + PS, ventilation with controlled pressure and guaranteed respiratory volume (up to) (Pressure-Controlled Ventilation Volume Guaranteed – PCV-VG), proportional auxiliary ventilation (Proportional Assist Ventilation – Pav + and Proportional Pressure Support Ventilation – PPS), Adaptive Support Ventilation (Adaptive Support Ventilation – ASV). In the settings of the device, there is a configuration of the backup ventilation mode, and it is possible to configure both inspiratory and expiratory triggers. Randomized studies have not showed advantages any regime in Nivl.Patients with sleepy apnea use Nivl in CPAP mode.2Standard Nivl Method:2– Set the reeer value 5 cm water.2– Choose the level of support for inspiratory pressure (PS, IPAP) individually by stepwise zoom from 5-8 cm water. Prior to reaching 6-8 ml per 1 kg due weight (DMT) (calculation of DMT (kg) is carried out according to the following formulas: Men = 50 + 0.91 × (growth, cm – 152.4), women = 45 , 5 + 0.91 × (growth, cm – 152.4). As a rule, this is achieved with a value of PS 10-16 cm water.2– establish the minimum sensitivity of the trigger, in which there is no autotriggy, – (-) 1.5 – (-) 2.0 cm water.st. For a pressure trigger, 2-3 l / min for a flow trigger.2– establish an inspiratory oxygen fraction in an inhaled gas mixture (FIO
) at a minimum level, which provides oxygen saturation of hemoglobin (SPO
– configure the sensitivity of the expiratory trigger to improve synchronization with the respirator (standard setting 25% is usually not suitable for patients with active inhalation attempts and when COPD, such patients should be installed 40-50% sensitivity),
– increase reeer to 8-10 cm water.st. In patients with spo
less than 88% on FIO background
0.3 when carrying reer increase.
High levels of PEEP / CPAP (> 12 cm water) and / or PS (> 20 cm water.
Reducing the front, as a rule, is achieved shortly after adjusting the adequate ventilation mode, while hypercapnia and / or hypoxemia correction can occupy several hours.
In the first hours, the auxiliary non-invasive ventilation of the lungs should be carried out in constant mode. Next, after a gradual decrease in respiratory support, it is possible to transition to Nivl sessions for 3-6 hours per day until its complete cancellation.
Recommendation 15.
It is recommended in the process of conducting the NIVL monitoring and evaluating the effectiveness of non-invasive ventilation of the lungs. With the ineffectiveness of mask ventilation, it is necessary to immediately intubate the trachea and start the invasive IVL (the level of evidence of evidence – 2, the level of persuasive recommendations – c).
Comments.
In the process of NIV, it is necessary to monitor the following parameters:2– the degree of leakage from the circuit;2— synchronization with the fan;
– blood pressure level and heart rate;2.
– participation in breathing of auxiliary respiratory muscles;
An hour after the start of NIV, it is necessary to evaluate the RR, TO (in liters), PaO
/FiO
, PaCO
. With an increase in RR, an increase in the ratio of RR / DO above 100, a decrease in PaO
/FiO
below 175 mmHg, increasing PaCO
NIV should be considered ineffective.
In most cases, the first day is the decisive period in determining the success of NIV. During this period, the patient should be under particularly careful monitoring. With the improvement of physiological parameters during the day, the probability of the effectiveness of NIV is high.
If there are criteria for the ineffectiveness of NIV, NIV should be stopped, the trachea intubated and ventilation continued through the endotracheal tube. The delay in tracheal intubation in this case leads to a worse prognosis.
NIV failure criteria:
1) the inability of the patient to transfer the mask due to discomfort or pain;
2) failure of mask ventilation to improve gas exchange or reduce dyspnea;
3) the need for endotracheal intubation to sanitize the secret of the tracheobronchial tree or protect the respiratory tract;4) hemodynamic instability;
5) myocardial ischemia or life-threatening arrhythmias;6) depression of consciousness or delirium;
7) increase in BH;
8) an increase in the ratio of BH / DO above 100;
9) PaO
/FiO below 175 an hour after the start of NIV;
10) increase in PaCO4. Non-invasive high-flow oxygenation
High-flow (high-speed) oxygen therapy (HFO) is a type of oxygen therapy, however, in most studies it is compared with NIV due to some similarities in physiological and clinical effects. Unlike NIV, when using HPE, it is impossible to create a controlled final expiratory pressure, control the inspiratory volume and minute ventilation of the lungs. At the same time, HPE has undoubted advantages over traditional oxygen therapy, it is more comfortable, and it does not have many disadvantages of NIV.
4.1. Equipment
VPO is implemented by means of a high-speed gas flow generator (up to 60 l/min and more). VPO includes various systems for efficient humidification and heating of the gas mixture. The main thing is the possibility of step-by-step regulation of the flow rate and temperature, precise setting of the oxygen fraction. Modern HPE systems have special breathing circuits made of a semi-permeable material that does not allow the formation of condensate, as well as original nasal or tracheostomy cannulas.4.2. Mechanisms of clinical efficacy of HPE
The basis of the clinical effectiveness of HPE is the possibility of creating a high gas flow rate (up to 60 l/min), which provides the following:— high gas flow rate, equal to or greater than the flow rate when the patient inhales, minimizes the "admixture" of room air and allows you to maintain a given high oxygen fraction [66];
– a high gas flow rate corresponds to a high gas velocity when inhaling patients with ARF, resulting in a decrease in respiratory rate, an increase in TO, this leads to a decrease in hypercapnia, a decrease in the work of breathing, an increase in oxygenation and a decrease in the degree of DN;
– high gas flow rate improves carbon dioxide elimination and alveolar ventilation, reducing the volume of anatomical dead space, which leads to a decrease in hypercapnia, a decrease in the work of breathing, an increase in oxygenation and a decrease in the degree of DN [67];
— high gas flow rate improves gas exchange by generating low (1–4 mbar) positive pressure in the hypopharynx and upper respiratory tract (CPAP-like effect) [68–70];
— high gas flow rate reduces the patient's work of breathing [71];
— positive respiratory effects of high gas flow rate are not accompanied by deterioration of cardiohemodynamics.
4.3. Indications for the use of HPE
Recommendation 16
In general, the indications for the onset of HPE correspond to the indications for NIV. The benefits of HPE over NIV have been demonstrated in patients with community-acquired pneumonia (LE: 2,уровень убедительности рекомендаций — В), гипоксемической ОДН при иммуносупрессии (уровень достоверности доказательств — 2, уровень убедительности рекомендаций — В), при кардиогенном отеке легких (уровень достоверности доказательств — 2, уровень убедительности рекомендаций — С), при обострении ХОБЛ и в профилактике постэкстубационной ОДН (уровень достоверности доказательств — 2, уровень убедительности рекомендаций — В).
Comments.
В мультицентровом рандомизированном исследовании, включившем пациентов с первичной патологией легких (внебольничная пневмония — более 60% пациентов, госпитальная пневмония) а также иммуносупрессией, продемонстрировано снижение частоты интубации трахеи и летальности при применении ВПО по сравнению со стандартной оксигенотерапией и НИВЛ [44]. В мультицентровом рандомизированном исследовании продемонстрировано снижение частоты интубации трахеи и летальности при применении ВПО не только по сравнению со стандартной оксигенотерапией, но и по сравнению с НИВЛ [55, 72].
У пациентов с кардиогенным отеком легких легкой и средней степени тяжести в рандомизированном исследовании продемонстрировано снижение частоты дыхания при применении ВПО по сравнению со стандартной оксигенотерапией [73].
У пациентов с ХОБЛ, получающих оксигенотерапию на дому, продемонстрировано уменьшение частоты обострений ХОБЛ при 6-часовом ежедневном использовании ВПО [74—76].2В рандомизированном исследовании у пациентов плановой хирургии с низкой степенью риска развития послеоперационной ДН в послеоперационном периоде продемонстрировано снижение частоты интубации трахеи при применении ВПО по сравнению со стандартной оксигенотерапией [77]. У пациентов в плановой кардиохирургии с развившейся после оперативного вмешательства гипоксемией продемонстрирована эквивалентность ВПО иНИВЛ в частоте интубации трахеи и летальности [78—80].
Рекомендация 17.
Рекомендуется использовать ВПО при ожидаемой трудной интубации трахеи и в паллиативной медицине (уровень достоверности доказательств — 2, уровень убедительности рекомендаций — С).
Comments. The clinical studies demonstrates the provision of adequate arterial oxygenation in patients with the trachea predicted difficult intubation (MalMampati Score, 2-4th degree) for 5-6 min [81, 82].
In patients receiving palliative care, it allows to reduce the degree of dance and avoid the use of Nivl [83].4.4. Algorithm application VPO
Recommendation 18.
When configuring it, it is necessary to use a specific algorithm (the level of evidence of evidence – 4, the level of persuasive recommendations – c).Comments.
Currently, there is no unambiguous opinion regarding the most optimal algorithm for selecting primary settings of the EHF and the subsequent correction of them in patients with DN of various genesis.The main criteria for using HPE are:
– Development of D.N. Of various genesis in the absence of indications for immediate intubation and the start of the IVL. – It should be started only after reaching the temperature of the gas mixture of at least 37 ° C and constantly monitor this indicator..
 – Under the manifestation of parenchymal OND, it is advisable to begin VPO with an oxygen fraction of 0.3-0.4.
– Under the manifestation of parenchymal OND, it is advisable to begin VPO with an oxygen fraction of 0.3-0.4.
– In the manifestation of parenchymathous one, it is advisable to begin with a low speed of the gas flow – 20-30 l / min, if necessary, followed by an increase in the flow rate.
– In the absence of effect, it is advisable to gradually increase the gas flow rate, focusing on the indicators of the gas exchange and the state of the patient.
– In the absence of effect, an oxygen fraction can be increased.
– With the development of hypercapnic OND, it is possible to begin at high speed of the gas flow – 50-60 l / min.
– At the stage of cessation of IVL, in an early post-spending period, it is possible to begin the high speed of the gas flow – 50-60 l / min. 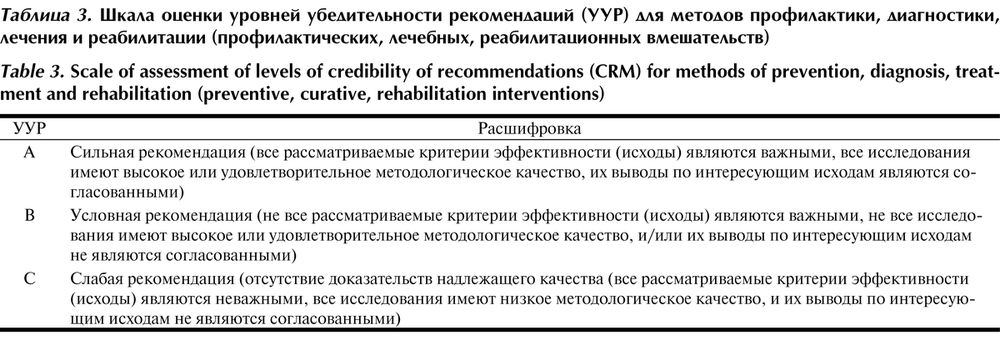 – Currently there are no clear recommendations for the termination of HPE. General Output algorithms from HPO are similar to the basic principles of reducing RP:
– Currently there are no clear recommendations for the termination of HPE. General Output algorithms from HPO are similar to the basic principles of reducing RP: 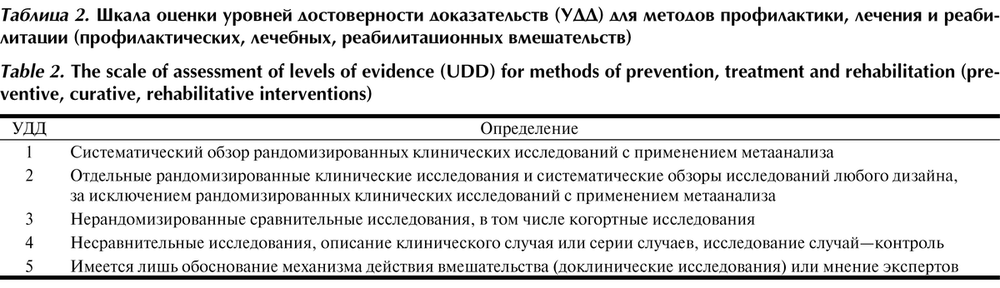 – A gradual decrease in the rate of gas flow – n5 l / min every 6-8 hours.
– A gradual decrease in the rate of gas flow – n5 l / min every 6-8 hours.
– transition to traditional hydrochiotherapy or spontaneous breathing at a gas flow rate ≤20 l / min and fio
<0.5 with adequate indicators of gas exchange and in the absence of signs of increasing DN.
– According to the readings, the periodic renewal of the VPO (sessions) at the stage of termination of the RP.
4.5. Contraindications to the use of VPO
Recommendation 19. « Currently, no significant adverse effects and complications are not described during the VPO (level of evidence of evidence – 4, the level of persuasiveness of recommendations is C). «Comments.» The simplicity of using the method and the "friendly" instrument interface minimize the potential possibility of errors as a result of the "human factor". Effective hydration and warming of the gas mixture provide the protection of the VF and the lungs. In patients with COPD, when using HAP with a high oxygen fraction, the respiratory acidosis is possible due to the decrease in the CHA and hypoventilation.
5. Rehabilitation and dispensary observation «Recommendation 20.».
It is recommended to rehabilitate patients receiving non-invasive ventilation (the level of evidence of evidence – 4, the level of persuasiveness of recommendations is C).
Comments. The main rehabilitation measures are aimed at regressing manifestations of DN and based on the general principles of patient management with acute or exacerbation of chronic DN..
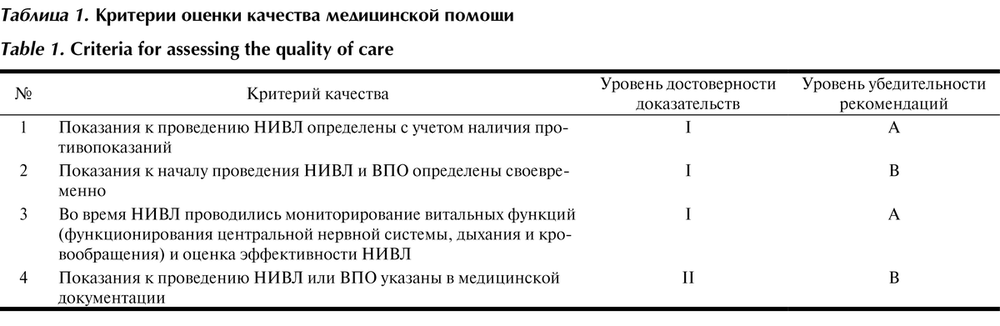
Criteria for assessing the quality of medical care are presented in
Table. one
Table 1. Criteria for assessing the quality of medical care
Appendix A2. Clinical Recommendation Development Methodology
Target audience of clinical recommendations:
1. Doctor anesthesiologist resuscitation.
2. Students of medical universities, residents, graduate students.
In these clinical recommendations, all information is ranked by the level of reliability (evidence) depending on the number and quality of research on this issue (Table 2, 3).
Table 3. Scale of estimating levels of persuasive recommendations (UUR) for the methods of prevention, diagnosis, treatment and rehabilitation (preventive, medical, rehabilitation interventions)
Table 2.Scale of evaluation levels of evidence (UDD) for the methods of prevention, treatment and rehabilitation (preventive, medical, rehabilitation interventions)
The procedure for updating clinical recommendations
Clinical recommendations are updated every 3 years.
Related documents
These clinical recommendations are designed to meet the following regulatory documents:
1. Order of the Ministry of Health of the Russian Federation of November 15, 2012 No. 919n
On approval of the procedure for providing medical care to the adult population by profile
Anesthesiology and resuscitation
(with changes and additions).
2. Order of the Ministry of Health of the Russian Federation of May 10, 2017 No. 203N
On approval of criteria for assessing the quality of medical care3. Order of the Ministry of Health of the Russian Federation of December 17, 2015 No. 1024N "On the classification and criteria used in the implementation of medical and social expertise citizens by federal government agencies of medical and social expertise."
The patient's management algorithm is represented in
Appendix B.
Appendix A1. Composition of the Working Group
Vlasenko A.V. – D.N., Professor of the Department of Anesthesiology and Emergency Medicine FGBOU DPO "Russian Medical Academy of Continuing Vocational Education" Ministry of Health of Russia.
Gritsan A.I. – D.M., Prof., Head of the Department of Anesthesiology and Resuscitation, IPO FGBOU VO "Krasnoyarsk State Medical University. Professor V.F. War-Yasenetsky "Ministry of Health of Russia, director of KGBOU DPO" Krasnoyarsk Regional Center for Advanced Training Specialists with Medium Medical Education ", President of the Krasnoyarsk Regional Association of Anesthesiologists and Resuscitations, Chief Freelance Specialist Anesthesiologist-Resuscitator Ministry of Health of the Krasnoyarsk Territory, Chief Freelance Anesthesiologist-Resuscitator of the Siberian Federal District , Vice-President of the All-Russian Public Organization "The Federation of Anesthesiologists and Resuscitations".
Kirov M.Yu.– Doctor of Medical Sciences, Prof., Head of the Department of Anesthesiology and Resuscitation of the Federal State Budgetary Educational Institution of Higher Education "Northern State Medical University" of the Ministry of Health of Russia. Kolesnichenko A.P. – Doctor of Medical Sciences, Prof., Professor of the Department of Anesthesiology and Resuscitation, IPO FSBEI HE “Krasnoyarsk State Medical University named after I.I. professor V.F. Voyno-Yasenetsky" of the Ministry of Health of Russia.Lebedinsky K.M. – Doctor of Medical Sciences, Prof., Head of the Department of Anesthesiology and Intensive Care named after A.I. V.L. Vanevsky Federal State Budgetary Educational Institution of Higher Education "North-Western State Medical University. I.I. Mechnikov" of the Ministry of Health of Russia.
Nikolaenko E.M. – Doctor of Medical Sciences, Prof., Head of the Center for Anesthesiology and Resuscitation of the NCHUZ “Scientific Clinical Center of the Open Joint Stock Company “Russian Railways”.Protsenko D.N. – Chief Physician of the Moscow State Budgetary Institution of Health “City Clinical Hospital No. 40” of the Moscow City Health Department, Candidate of Medical Sciences, Associate Professor, Head. Department of Anesthesiology and Resuscitation, Federal State Budgetary Educational Institution of Higher Education "Russian National Research Medical University. N.I. Pirogov" of the Ministry of Health of Russia, member of the Presidium of the All-Russian Public Organization "Federation of Anesthesiologists and Resuscitators".
Yaroshetsky A.I. – Doctor of Medical Sciences, Head of the Department of Anesthesiology and Resuscitation of the Research Institute of Clinical Surgery of the Federal State Budgetary Educational Institution of Higher Education Russian National Research Medical University named after I.I. N.I. Pirogov" of the Ministry of Health of Russia.
Appendix B. Patient Information
Respiratory diseases are very common. There is strong evidence to support the use of non-invasive ventilation in patients with acute respiratory failure secondary to exacerbation of chronic obstructive pulmonary disease, acute cardiogenic pulmonary edema, or immunosuppression. In addition, the use of non-invasive ventilation reduces the rate of unsuccessful extubations in patients with chronic obstructive pulmonary disease.

